Vara’s full-stack bet for real-world evidence at an unprecedented scale
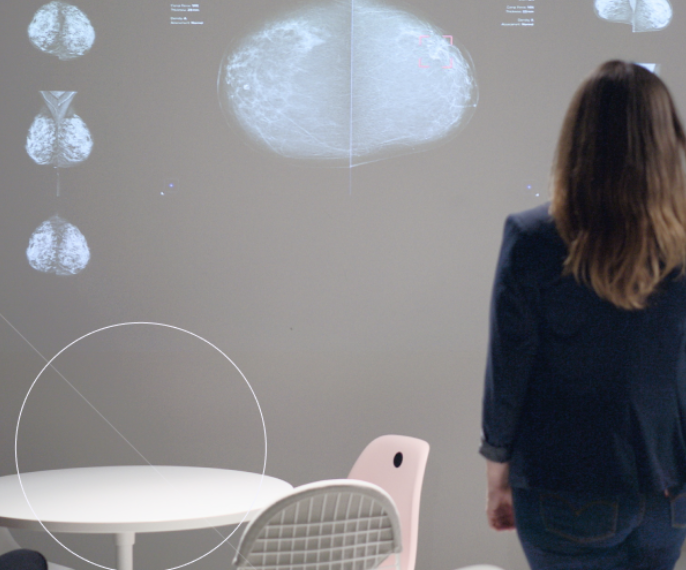
30% of all screening centres in Germany actively use the Vara platform and we’re the first company in the world with large-scale real-world evidence from clinical routine. This comes down to our full-stack approach: We’re reimagining the entire workflow instead of integrating AI as a standalone plug-in.
Our ambition at Vara is to find every deadly breast cancer early, such that more women survive. AI is a powerful tool that helps us achieve this goal, but it’s only a means to an end.
Recent history has shown that AI, on its own, is no silver bullet. It is not enough to build an AI model that takes mammograms and outputs a cancer score. AI alone can’t solve the problems surrounding breast cancer diagnoses and it can’t magically deliver value straight out of the box.
This narrow focus is what first-generation AI companies in this space got wrong. And it’s the reason why, for all its promises, AI is yet to move the needle when it comes to breast cancer cases.
To unleash AI’s transformative potential, we have to build an entirely reimagined clinical workflow. We have to go “full-stack”.
The full-stack approach
What does full-stack mean in the context of AI for breast cancer screening? Here is what we believe are the three necessary components:
1. An AI-first, web-based reporting workflow designed for radiologists:
Many AI models for medical imaging integrate into existing, old workflow tools or outdated PACS viewers. By retrofitting such new technologies into such old programs, a ton of potential is left on the table.
A modern, web-based workflow layer itself creates much more value because it consolidates the previously fragmented process in one place. It creates structured reports, enables remote collaboration, and brings efficiency to the workflow. Its superior UX drives adoption and motivates screening radiologists to contribute data and expert knowledge to AI development.
Most importantly, Vara’s proprietary workflow is designed to perfectly leverage AI to create a new clinical workflow. Our AI automates repetitive work by preparing fully pre-written medical reports. Or it interferes when a screening radiologist has missed a particularly suspicious lesion. AI filters the worklist and gives radiologists the chance to get control over their workday by focusing on the more difficult cases when they feel most ready for it.
2. Radiologist-AI interaction and feedback loop:
Our full-stack workflow gives us another important edge over plug-ins that are integrated into incumbent software. We can finetune the way AI and individual radiologists interact.
No two radiologists behave the same, especially in a tricky domain like breast cancer screening, and there is a good deal of ambiguity. Radiologists tend to be over-readers (too many false positives) or under-readers (too many false negatives). A one-size-fits-all AI model doesn’t do this diversity justice. At Vara, we fine-tune the model for each radiologist, in order to optimise for joint performance of radiologist and AI.
And because longitudinal and biopsy data is fed back to Vara, we can provide each radiologist visibility on how their performance has improved over time with Vara and where they tend to disagree with Vara. That creates high excitement with radiologists as we are jointly improving their expertise and our model over time.
3. Real-world evidence at population health scale:
History books are full of AI models that worked retrospectively but failed to show impact prospectively in new settings. Generalisation has to be repeatedly proven again in each new market. Also, it is not enough to have good performance on average. This performance needs to carry through into relevant subgroups like high breast densities or especially aggressive cancers.
A strictly data-driven approach is therefore necessary. For each woman diagnosed via Vara, we follow the patient pathway after screening to assess AI’s impact on population health metrics such as recall rates, biopsy scores and mortality. This data feedback loop from prospective clinical use allows us to constantly improve our AI models.
Harnessing AI’s transformative potential on a global stage
Measuring our effect on screening metrics at scale is possible because we are building not just the AI, but a full-stack workflow. Our data infrastructure allows us to continuously collect real-world evidence in the clinical routine — for the first time globally.
In the future, this infrastructure can be used to improve breast cancer screening even further, for example by adjusting the screening interval based on individual risk, or even stratifying the treatment itself. The data collected will allow regulators and policymakers to accurately assess the impact and make quick, rational, data-driven decisions to further improve the standard of care.
Beyond Germany, a full-stack platform is inevitable to democratise access to breast cancer screening and launch 1,000 screening centres everywhere in the world. It is the infrastructure for safe, data-driven, effective and affordable screening!
---
This article is a part of the vara.ai Founder's Blog, where the leadership team of Vara share insights to their journey. Follow the Founders Blog here.
Read more

Mar 2, 2023


